If you are an adult male, it’s normal as you get older to have less testosterone in your body. The male sex hormone testosterone plays a critical role in, among other things, sexual desire and arousal. Therefore, it’s not surprising that as men experience decreases in testosterone levels, one of the noticeable effects they experience is decreased sex drive and increased sexual function issues.
This can lead many men to seek out treatments and therapies, such as testosterone replacement therapy, to attempt to regain the same kind of sex drive, stamina, and so on that they had in their youth. Alternatives to testosterone replacement therapy, such as lifestyle modifications, dietary changes, and herbal supplements, may also be considered by those seeking to address age-related changes in testosterone levels.
One of the medically-approved ways to improve testosterone levels is with testosterone replacement therapy. However, this is not usually prescribed for age-related testosterone loss, but rather for low testosterone levels caused by other medical conditions or pathologies. It comes with great risks for many patients as well. The good news is there are several other therapies available, all of which work in different ways. Some have a high degree of risk associated with them or are considered off-label use. Others may boost libido, sex drive, and sexual performance capabilities with little risk.
Below, we’ll briefly talk about testosterone replacement therapy, and then examine some of the alternatives to testosterone replacement therapy that men should consider for similar or better outcomes with fewer side effects or risks.
Table of Contents
Testosterone Loss Due To Aging
Most men are aware that their testosterone levels naturally decrease over time as they age. This is backed up by science – on average, from the time men reach their mid- to late-30s, their levels of testosterone production drop by around 1% per year, or 10% per decade (Feldman et al, 2002). This is one of the contributing factors to a decrease in libido, increase in sexual function issues and erectile dysfunction, and the associated psychological and relationship issues that can develop in men as they age. Despite this, it’s considered a normal part of aging. But, that doesn’t mean that men have to simply accept this change, and can’t do anything about it.
There are a variety of treatments as well as lifestyle changes that can be made to boost energy levels, libido, stamina, and related traits. The first and most direct is by boosting testosterone levels with testosterone replacement therapy. That comes with a lot of risks, however, and while we won’t go into great detail here, we’ve covered those risks and side effects in separate articles on testosterone replacement therapy.

Testosterone Replacement Therapy Is Not Usually Prescribed For Age-Related Loss
Even for men who consider the risks associated with testosterone replacement therapy to be worthwhile, it may not be that simple. In most cases, doctors will not prescribe or consent to testosterone replacement therapy simply for age-related testosterone decline. It’s almost exclusively reserved for treating what is formally known as hypogonadism – an abnormally low testosterone level for the patient’s age, often resulting from medical conditions, illnesses, disease, congenital disabilities, or other endogenous causes.
Testosterone replacement therapy usually consists of a gel, injection, implanted capsule, or another mechanism for allowing the testosterone to be absorbed into the body and boost circulating testosterone levels. Each of the various methods used for testosterone replacement therapy has its own risk/reward profiles, on top of the inherent risks associated with testosterone replacement therapy. In general, simply supplying replacement hormones to the body is seen as high risk, whether in the form of testosterone or any other substances that are so critical for so many biological processes (Osterberg et al. 2014).
Other Sex Hormone Treatments
There are other sex hormone treatments, which aim to improve testosterone levels directly or indirectly, but without using testosterone itself. These have varying evidence for their efficacy, and only the first highlighted below is used for treating hypogonadism. In all cases, none of these treatment options are considered approved or on-label for boosting testosterone levels that have declined due to aging. That can make them difficult to impossible for most men to obtain explicitly for that purpose. For more information on these specific treatments, to discuss with your doctor, you can read this excellent literature review paper on the topic.

Human Chorionic Gonadotropin
Human chorionic gonadotropin, or hCG, is a compound that is found within the placenta of pregnant women, and is chemically homologous to lutenizing hormone. This hormone plays important roles during the fetal development, triggering, among other things, testosterone production in male babies. It has been shown to be effective in stimulating testosterone production in a certain class of cells within the testes of adult men suffering from hypogonadism.
However, as with most of these treatments, it is not generally prescribed or approved for age-related testosterone loss. The long-term safety and health risks associated with hCG therapy have not been well-established. Unlike pure testosterone replacement therapy, however, hCG has been shown to maintain or trigger the production of sperm, allowing men to retain their fertility – something that is often inhibited in testosterone replacement therapies.

Aromatase Inhibitors
Aromatase is an enzyme that is responsible for breaking down testosterone into estradiol in the body. Aromatase inhibitors, as their name suggests, inhibits the action of this enzyme. This results in both direct and indirect increases in the testosterone levels in the body. Though effective, this treatment for testosterone therapy is considered off-label use. Treatment for low testosterone has been shown to cause side effects, including hot flashes, weight gain, insomnia, joint aches, low bone mineral density/osteoporosis, and similar problems. On the upside, they are available via oral medications, rather than injection or other application methods common to most other forms of treatment. Long-term use for low testosterone and the associated side effects and risks have not been established.
Selective Estrogen Receptor Modulators
Selective estrogen receptor modulators, or SERMs, act as either antagonists or agonists on estrogen receptors (tissue-dependent). For our purposes, they act as estrogen receptor antagonists in the pituitary gland and hypothalamus, and thus prevent the normal inhibitory effects of estrogen on other sex hormones. The net result is an increase in testosterone levels, with spermatogenesis stimulated as well. It is currently used as an off-label medication for the treatment of hypogonadism.
Much like our other treatments, however, it is not typically prescribed for age-related testosterone loss treatment. Specifically, clomiphene citrate is usually used for this purpose, and provided in oral pills of 25 mg or 50 mg strength daily. Typical side effects include headache, dizziness, and fatigue. Long-term risks and side effects have not been established. Higher dosages may result in lower sperm counts, however.

Lifestyle Changes
Non-medication treatment options for low testosterone, both naturally-occurring from aging and occurring due to other medical pathologies, are also viable. These can work whether or not you are on testosterone replacement therapy or one of our alternative options. Many of the following lifestyle changes have been shown to not only increase testosterone production and libido, but provide numerous other benefits as well. In many cases, however, it is not clear if the lifestyle change alone results in the positive benefits, or serves to reduce or modify other health and medical conditions themselves, which then provide the benefits. In any case, these lifestyle changes include:
- Eating a healthy, well-balanced diet. This is key to maintaining a healthy weight, low body fat percentage, and sufficient lean muscle mass. Additionally, it is essential to managing potential health conditions that develop with age and reducing your risk for them. Obesity, diabetes, and similar conditions can depress libido and decrease testosterone levels in the body.
- Exercising regularly throughout your life. Adults need 2 to 3 hours of moderate exercise each week to remain healthy. Staying active increases muscle mass, helps keep weight in check, boosts the immune system, and can help increase testosterone production in men.
- Get 7 to 8 hours of good quality, restful sleep every night. Sleep plays a key role in regulating all of the hormones and their production in your body, and that includes the sex hormones.
- Address any underlying health problems and/or medication side effects with your doctor. Many medical conditions and medication side effects can result in decreased testosterone or depressed sexual function.
- Address any mental health and/or relationship issues with professionals, as these can artificially depress your libido and may be the cause of sexual health issues rather than any physical problem.
- Vitamin D has been shown to increase testosterone production, so be sure you are getting sufficient vitamin D in your diet or through supplements (around 3,300 IUs daily) (Pilz et al., 2010).
- Caffeine in moderation has been shown to boost testosterone, so have an extra cup of coffee each day.
- Low zinc levels can cause low testosterone, so be sure to take a supplement or multivitamin that includes your recommended daily intake of zinc (Prasad et al., 1996).
Treatment with a Non-Testosterone Option: Enclomiphene
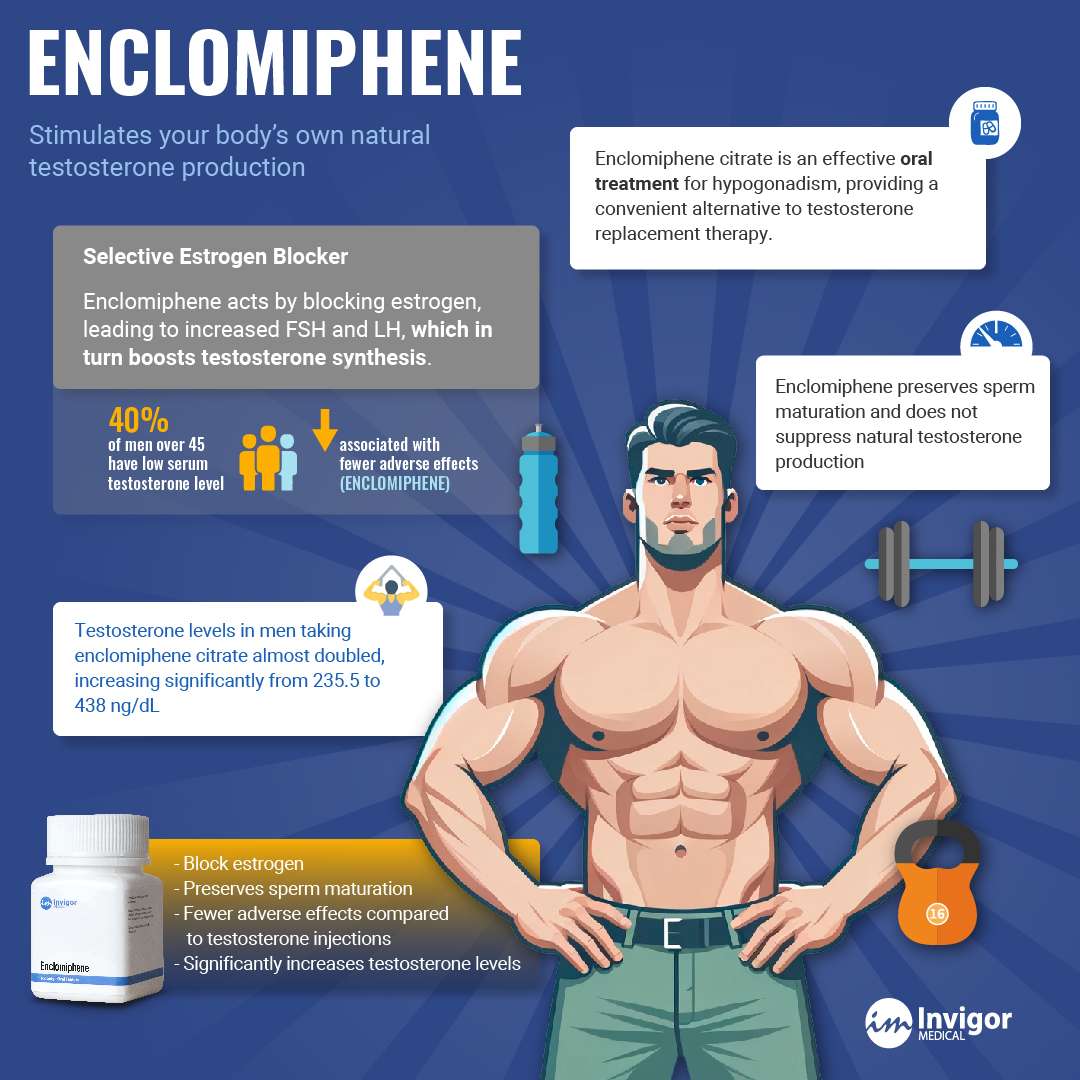
There is one treatment option that stands apart from traditional testosterone replacement therapies—it doesn’t introduce external testosterone into the body. Instead, it works by stimulating your body’s own natural testosterone production. This medication is called Enclomiphene, a selective estrogen receptor modulator (SERM) that’s gaining popularity as a non-hormonal alternative to TRT.
Enclomiphene increases natural testosterone by blocking estrogen receptors in the brain, which prompts the pituitary gland to produce more luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones, in turn, stimulate the testes to produce testosterone. This approach preserves fertility and avoids the common suppression of the hypothalamic-pituitary-gonadal (HPG) axis that occurs with direct testosterone therapy.
Because Enclomiphene works with your body’s hormonal signaling rather than overriding it, it may carry fewer long-term risks and side effects than traditional TRT. Many users report benefits such as improved energy, mood, libido, muscle mass, cognitive function, and sperm production—all without the need for external testosterone.
Concluding Thoughts on Alternatives to Testosterone Replacement Therapy
Several alternatives to testosterone replacement therapy are available, each with its own pros and cons. While many hormonal treatments carry potential side effects and involve off-label use, Enclomiphene stands out as a safe, effective, and fertility-preserving option. By enhancing your body’s own ability to produce testosterone, it offers a more natural path to restoring vitality, libido, and overall well-being.