The field of microbiology has witnessed significant advancements in recent years, particularly in our understanding of the microorganisms that inhabit the human body. Two terms that are commonly used in this context are microbiota vs. microbiome. While these terms are often used interchangeably, they have distinct meanings and refer to different aspects of the microbial world within us.
Table of Contents
What is the Microbiota?
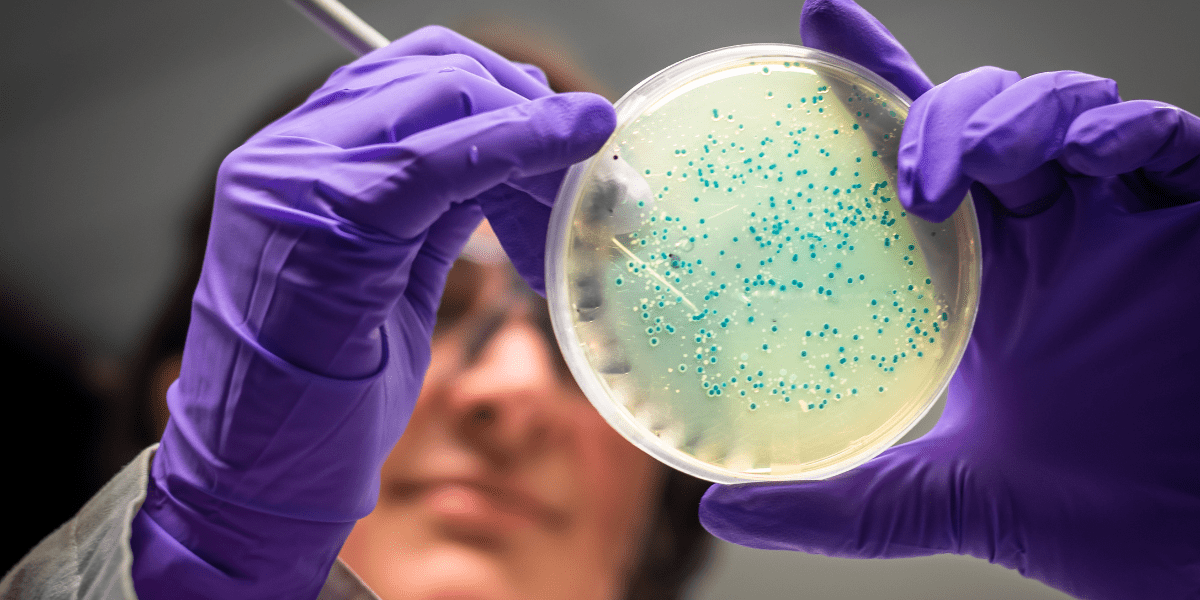
The term microbiota refers to the actual population of microorganisms that inhabit a specific environment, such as the human body. It includes bacteria, fungi, viruses, algae, archaea, and small protists that coexist within a particular ecosystem, like the human gut.1
In the past, it was controversial whether to include genetic elements such as viruses in the microbiota. The currently accepted definition of microbiota is the assemblage of living organisms in a defined environment.
Since genetic elements such as phages, viruses, plasmids, prions, viroids, and free DNA are not considered to be living microorganisms, they are not included in the microbiota.1
What is the Microbiome?
The term microbiome refers to the collective genetic material of the microorganisms that reside within a particular environment. It includes the genomes of all organisms and the microbial structural elements, metabolites, and environmental conditions in which the microbes live.
In the context of the human body, the microbiome encompasses the genes of the microorganisms that make up the human microbiota. The human microbiota contributes over 150 times more genetic information than humans.2
The host’s molecules, the metabolites that microbes produce, such as signaling molecules, toxins, and organic and inorganic molecules, as well as the surrounding environmental factors, are also part of the microbiome.1
Genetic elements such as phages, viruses, plasmids, prions, viroids, and free DNA are included in the microbiome but not the microbiota.
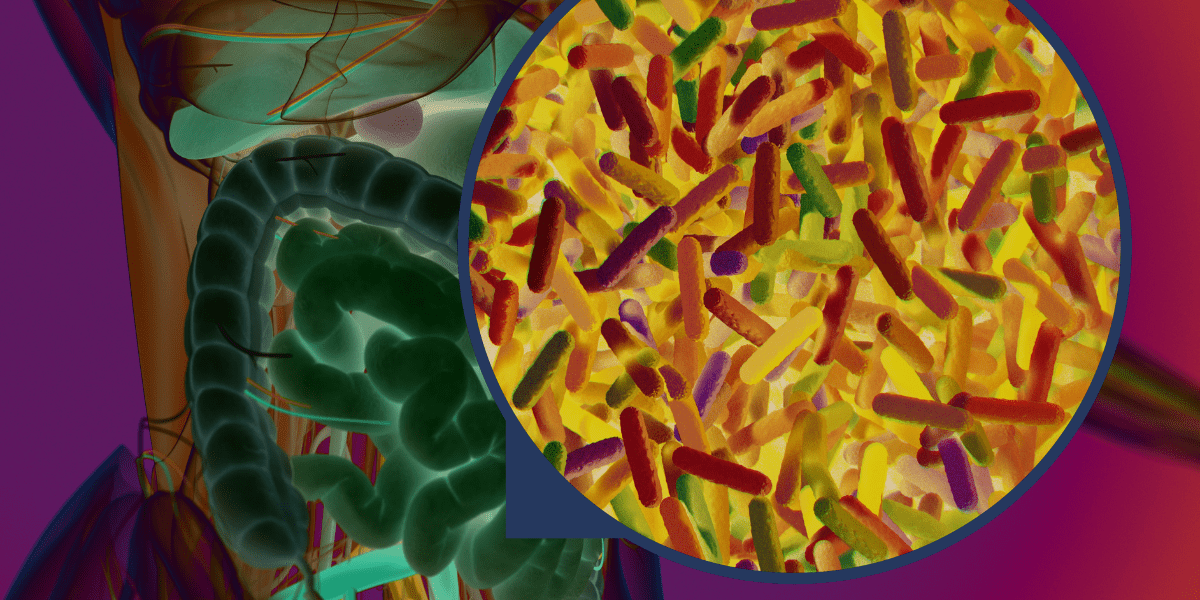
The Gut: Home for the Microbiome
The gut refers to the entire digestive system, from the mouth to the anus. The mouth, esophagus, and stomach lead into the small and large intestines. Most of the gut microbiota live in the large intestine, especially in a large outpouching called the cecum.
The large intestine is coated with a thick layer of mucus that separates the lumen of the large intestine, where the microbes live, from the intestinal wall and the bloodstream on the other side. Tight junctions join the cells in the large intestine, and immune cells reside in the wall of the large intestine. These are protections to keep the microbiota from causing disease.
The small intestine is coated with a much thinner mucous layer.
The Gut Microbiota: A Complex Ecosystem
Among the different microbial communities within the human body, the gut microbiota is of particular importance. The gut bacteria ferment food, protect against pathogens, stimulate the immune response, and produce vitamins.3
Generally, the gut microbiota is composed of six phyla, including:2
- Actinobacteria
- Bacteroidetes
- Firmicutes
- Fusobacteria
- Proteobacteria
- Verrucomicrobia
Firmicutes and Bacteroidetes are the major types. Lactobacillae, Streptococci, and Enterobacteria are also common in the gut.2 Overall, the human gastrointestinal tract contains over 100 trillion microorganisms.4 The diversity of gut bacteria increases between childhood and adulthood and decreases over age 70. Each person’s gut microbiome is unique and changes over their lifetime.2

The Microbiota is Ever-Changing.
Humans and their microbiomes evolve together throughout their lifetimes. Gut microbiomes vary between populations and between generations.
For example, Helicobacter pylori was the dominant microbe in the stomachs of almost all people in the early twentieth century. This bacterium disappeared in just 100 years. Today, H. pylori is a risk factor for peptic ulcers and stomach cancer. Losing these bacteria is associated with asthma, hay fever, and skin allergies in childhood.1
When researchers compared the microbiome samples from people living in the United States to those from less developed nations, such as Guahibo Amerindians and Malawians who consume a diet rich in maize, they found that U.S. adults have much less gut diversity. The Ameridians and Malawians had an increase in enzymes needed to break down plant polysaccharides, and U.S. adults had increased enzymes to break down simple sugars.5
Various factors, including diet, lifestyle, medications, and host genetics, influence the composition of the gut microbiome. Consuming a high-fat or high-sugar diet changes the ratio of microbes in the gut, as does consuming a Mediterranean or ketogenic diet.2
A plant-based diet does not perturb the microbiome as much as an animal-based diet does. A change in diet also changes the products produced by the microbes.6 These changes can increase or decrease the risk of disease.
The Significance of Microbiota vs. Microbiome for Human Health
The human microbiota and microbiome have far-reaching implications for human health. They are involved in numerous physiological processes, including digestion, metabolism, immune function, and even brain activity.
Microbiota secrete molecules that can have effects throughout the human body. Some of these molecules include:
- Bile acids
- Uric acids
- Short-chain fatty acids
- AHR ligands
- Catecholamines
- Histamine
- Prostaglandins
These molecules help regulate your innate and adaptive immune systems. They can have a significant effect on whether you develop a disease or medical condition in your lifetime.
The delicate balance of microorganisms within the body is essential for maintaining overall health and preventing the onset of various diseases.
The Role of the Microbiota vs. Microbiome in Disease and Health
The gut-brain axis is a two-way communication system between the gut and the brain. The microbiome is an integral part of our physiology that contributes to health and disease.
Factors that impact the gut-brain axis include:2
- Genetics and epigenetics
- Diet
- Mode of delivery at birth
- Environmental factors
- Drugs
- Exercise
Examples of how the microbiome affects brain neurophysiology include: 2
- Food intake
- Cognitive behavior
- Parkinson’s disease
- Mood
- Stress
- Social interaction
Emerging research has revealed that alterations in the composition and diversity of the human microbiome are associated with various diseases, including gastrointestinal disorders, obesity, autoimmune conditions, and mental health disorders.
Disorders associated with microbial perturbation in the gut include:2
- Depression
- Anxiety
- Autism spectrum disorder
- Parkinson’s disease
- Alzheimer’s disease
- Chronic obstructive pulmonary disease (COPD)
- Obesity
- Diabetes
- Cancer
- Cavities and oral health
- Cardiovascular disease
- Asthma
- Pneumonia
- Rheumatoid arthritis
- Inflammatory bowel disease
- Heart disease
- Liver disease
- Chronic kidney disease
Imbalances in the gut microbiota, known as dysbiosis, can disrupt the delicate ecosystem of microorganisms and contribute to the development of disease.
Understanding the role of the microbiome in disease pathogenesis opens up new avenues for therapeutic interventions and personalized medicine.
The Human Microbiome Project
To gain a deeper understanding of the human microbiome, the Human Microbiome Project (HMP) was initiated by the National Institutes of Health (NIH) in 2008. The goal of the project was to characterize the microbial communities inhabiting the human body and to explore their relationship with human health and disease.
The HMP provided valuable insights into the diversity, composition, and function of the human microbiome across different body sites. They list some of their major accomplishments:
- Sequencing 3,000 bacterial genomes isolated from the human body
- Profiling the human microbiome from 300 people
- Completing one complete dataset of the bacterial, fungal, viral, and protist community
Microbiome Testing
Advances in sequencing technologies have made it possible to analyze the composition and function of the human microbiome in greater detail. Microbiome testing, also known as microbiome profiling, involves the collection of samples from different body sites, such as the gut or skin, followed by DNA sequencing to identify and quantify the microorganisms present. This type of testing provides valuable information about the diversity and abundance of microbial species, allowing for personalized approaches to healthcare and disease management.
The Future of Microbiota vs. Microbiome Research
Due to advancements in sequencing technologies, analytical techniques, and computational tools, the field of microbiome research is rapidly evolving. A greater understanding of microbiota vs. microbiome is leading to better treatments to support the microbiome.
Future research aims to uncover the intricate relationships between the microbiota vs. microbiome and various aspects of human health, such as immune function, metabolism, and mental well-being.
Additionally, the development of targeted interventions and therapeutics that modulate the microbiome holds promise for the treatment and prevention of a wide range of diseases. For example, fecal microbiota transplants are used to restore a healthy microbiome in patients with Clostridium difficile infection.
The gut produces the hormone GLP-1. The microbiome impacts GLP-1 hormone production. Research suggests that the microbiome impacts your risk of weight gain and obesity. Medications such as the semaglutide supplement GLP-1 reduce appetite and food cravings and lead to significant weight loss. If you have questions about semaglutide, contact a treatment specialist at Invigor Medical.